Understanding RFI and RFP in Healthcare Procurement
Unlock the RFP process in healthcare. Understand its role, challenges, and best practices. Elevate procurement strategies. Click to learn more!

Procurement isn't just a back-office task in healthcare; it directly impacts patient care, safety, and operational efficiency. When hospitals select the wrong vendor or delay critical purchases, the consequences ripple across clinical outcomes, compliance risk, and financial performance.
We understand how challenging and high-pressure managing procurement processes can be, especially when patient care and compliance hang in the balance. That's why structured, transparent procurement processes matter.
So, if you're a healthcare vendor or part of a hospital's procurement team, you've likely worked with RFIs and RFPs. However, here's the reality: many people still struggle to clarify their purpose, timing, and how to manage them effectively.
So, what is RFP in healthcare? And where does an RFI fit into that process? More importantly, how can vendors respond faster, and how can procurement teams cut review times without compromising quality or compliance?
In this blog, you'll get clear, actionable answers. We'll break down the role of RFIs and RFPs in healthcare procurement, show you their key differences, and address common challenges and best practices to manage these processes smarter and faster.
TL;DR
- RFIs (Requests for Information) help healthcare organisations explore market options and vendor capabilities early in the procurement process.
- RFPs (Requests for Proposals) formally invite vendors to submit detailed, competitive bids for specific projects, such as EHR systems or imaging equipment.
- Traditional healthcare RFI/RFP processes are slow, involve extensive compliance requirements, and often experience delays due to siloed teams and manual document handling.
- Common RFP pitfalls include incomplete documentation, vague security protocols, and overlooked state-specific laws, which can delay decisions or disqualify bids.
- AI-powered platforms like Inventive AI automate proposal generation, enforce built-in HIPAA and FDA compliance, and cut RFP cycle times by up to 70%.
- Adopting AI-driven procurement tools ensures faster, fairer, and more accurate vendor selection in healthcare's highly regulated environment.
What is an RFI in Healthcare Procurement?
In healthcare procurement, getting/giving the correct information early can save your organisation time and money. This is where a Request for Information (RFI) plays a critical role.
An RFI is a formal document to collect preliminary details about potential vendors, services, or technologies. It helps gather insights before making a purchasing decision. Think of it as a structured way to understand what the market offers without committing to any vendor.
Why Use an RFI?
The primary goal of an RFI is to support market research. Clients use it to explore new solutions, discover vendor capabilities, or evaluate available technologies. In healthcare, this often applies when they're considering:
- New medical equipment or devices
- Healthcare IT systems or software solutions
- Facility management or tele-health services
- Specialised clinical service providers
For example, if a hospital is exploring advanced imaging equipment but isn't ready to request bids, an RFI can help gather specifications, pricing ranges, and vendor qualifications.
Structure of a Typical Healthcare RFI
A well-crafted RFI typically includes these sections:
- Introduction: A brief overview of your organization and project context.
- Information Requested: A list of specific questions or data you need from vendors.
- Response Guidelines: Instructions on how vendors should submit their responses.
- Timelines: Deadlines for submissions and next steps.
RFIs are intentionally broad. They aren't meant to finalize a deal but to support informed decision-making before proceeding with a Request for Proposal (RFP).
Key Benefits of an RFI
Using RFIs in your procurement process delivers several advantages:
- Saves Time: Clients can quickly filter out vendors who don't meet basic requirements.
- Promotes Transparency: Standardised questions ensure fair, consistent information gathering.
- Clarifies Scope: You define what you need before writing an RFP, avoiding delays and revisions.
What is an RFP in Healthcare Procurement?
If you're a healthcare vendor or solutions provider, understanding how procurement teams manage RFPs is essential. A Request for Proposal (RFP) is a formal, structured document healthcare organizations use to solicit competitive bids. It signals that a hospital or health system is ready to review detailed solutions and select the most suitable partner.
Why Procurement Teams Use RFPs
An RFP helps healthcare organizations find vendors that meet their technical, financial, and compliance standards. You can present a complete, tailored proposal addressing their needs as a vendor.
When you grasp what is RFP in healthcare, you position your response to meet expectations and increase your chances of being selected.
What Does a Healthcare RFP Typically Include?
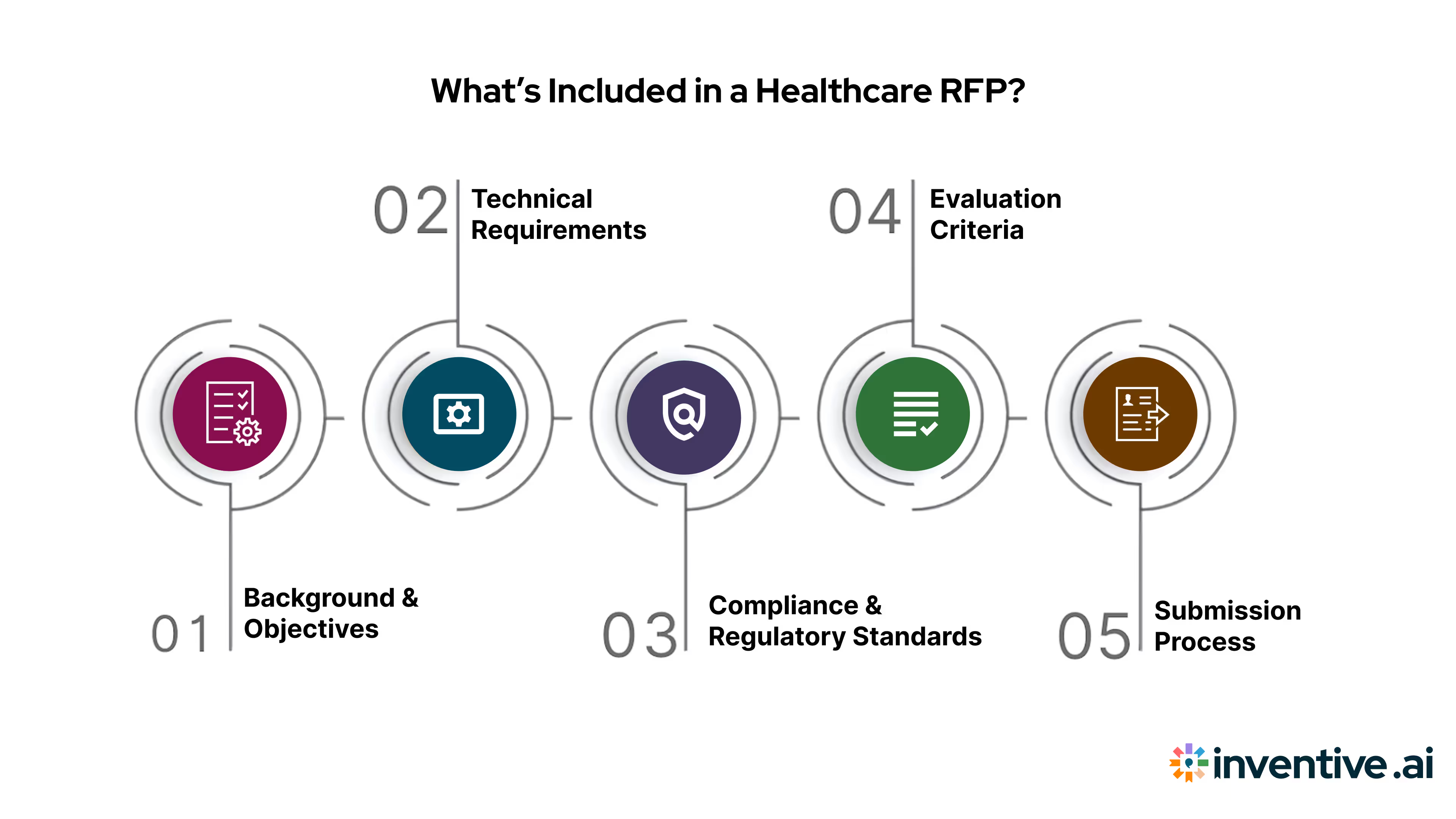
Healthcare procurement teams expect specific, structured responses. Here's what you'll usually find in an RFP:
- Background & Objectives: Context about the healthcare facility and the project's purpose.
- Technical Requirements: Detailed system specs, integration needs, and performance benchmarks.
- Compliance & Regulatory Standards: Requirements like HIPAA, FDA, HITRUST, and local health regulations.
- Evaluation Criteria: Clear guidelines on how proposals will be scored and evaluated for comparison.
- Submission Process: Instructions, response deadlines, and points of contact.
As a vendor, reviewing each section carefully ensures your proposal addresses every requirement and stands up to structured evaluation.
8 Types of RFPs in Healthcare You Should Know About
The most common healthcare RFP types include the following:
1. Healthcare IT & EHR RFPs
These RFPs focus on technology solutions such as Electronic Health Records (EHR) systems, telehealth platforms, patient portals, cybersecurity, and data integration tools. They emphasize interoperability, HIPAA compliance, data security, and vendor support models.
2. Medical Equipment & Device RFPs
Hospitals issue these RFPs to procure diagnostic machines, surgical instruments, imaging systems, monitoring devices, and other clinical equipment. Vendors must meet strict safety standards, maintenance requirements, and regulatory approvals.
3. Clinical Services RFPs
These RFPs request outsourced medical services ranging from radiology and pathology to rehabilitation, urgent care staffing, and specialty clinic management. Evaluation often focuses on clinical quality, certifications, staffing models, and patient outcomes.
4. Pharmacy & Medication Management RFPs
Health systems release pharmacy-related RFPs for medication distribution, formulary management, specialty pharmacy services, and drug procurement. These RFPs require detailed information about compliance, auditing processes, and cost-containment strategies.
5. Healthcare Consulting RFPs
Hospitals frequently seek consulting expertise for operational improvement, revenue cycle management, digital transformation, risk assessment, and compliance audits. These RFPs evaluate methodology, past performance, and industry experience.
6. Facility Construction & Renovation RFPs
Large healthcare networks issue RFPs for hospital expansions, new clinics, laboratory construction, or modernization projects. These documents focus on architectural design, engineering experience, safety standards, and regulatory alignment.
7. Health Insurance & Benefits RFPs
Employers and healthcare organizations issue RFPs for employee health plans, third-party administrators (TPAs), wellness program providers, and claims management services. Cost structure, coverage flexibility, and administrative support are key evaluation areas.
8. Public Health & Community Program RFPs
Government agencies and nonprofits issue these RFPs to support vaccination programs, mental health initiatives, data research projects, and community outreach services. They prioritize impact measurement, reporting capabilities, and scalability.
Common Scenarios for RFPs in Healthcare
You'll encounter RFPs for a wide range of healthcare needs, such as:
- Electronic Health Record (EHR) platforms
- Imaging and diagnostic equipment
- Facility operations management services
- Telehealth and patient engagement solutions
For example, if a hospital seeks to implement a new EHR, it will issue an RFP detailing integration with existing systems, security protocols, and regulatory needs. You'll be expected to respond with a comprehensive, compliant proposal.
Why RFPs Matter for Vendors
An RFP isn't just a paperwork exercise; it shapes how your solution is evaluated. Here's why responding well matters:
- Ensures Accountability: Your proposal becomes part of an official vendor record.
- Supports Comparative Evaluation: Procurement teams use consistent criteria to compare your response directly against competitors.
- Helps Align Your Solution: Detailed RFPs show you precisely what a healthcare client values, letting you tailor your offer.
Understanding what is RFP in healthcare helps you respond faster, reduce errors, meet regulatory expectations, and recognize that proposal success may depend on overcoming subjective, error-prone processes with proper tools.
Curious how to improve your RFP responses and cut proposal errors? Inventive AI auto-generates HIPAA-compliant, audit-ready responses in minutes. Explore how it works.
With a clear picture of what both RFIs and RFPs offer, it's time to compare them and see when each is appropriate in healthcare procurement.
Step-by-Step Guide on Writing RFPs in Healthcare
The following steps outline how hospitals, clinics, payers, and public health organizations can structure a high-quality RFP that attracts qualified vendors and supports safe, cost-effective decision-making.
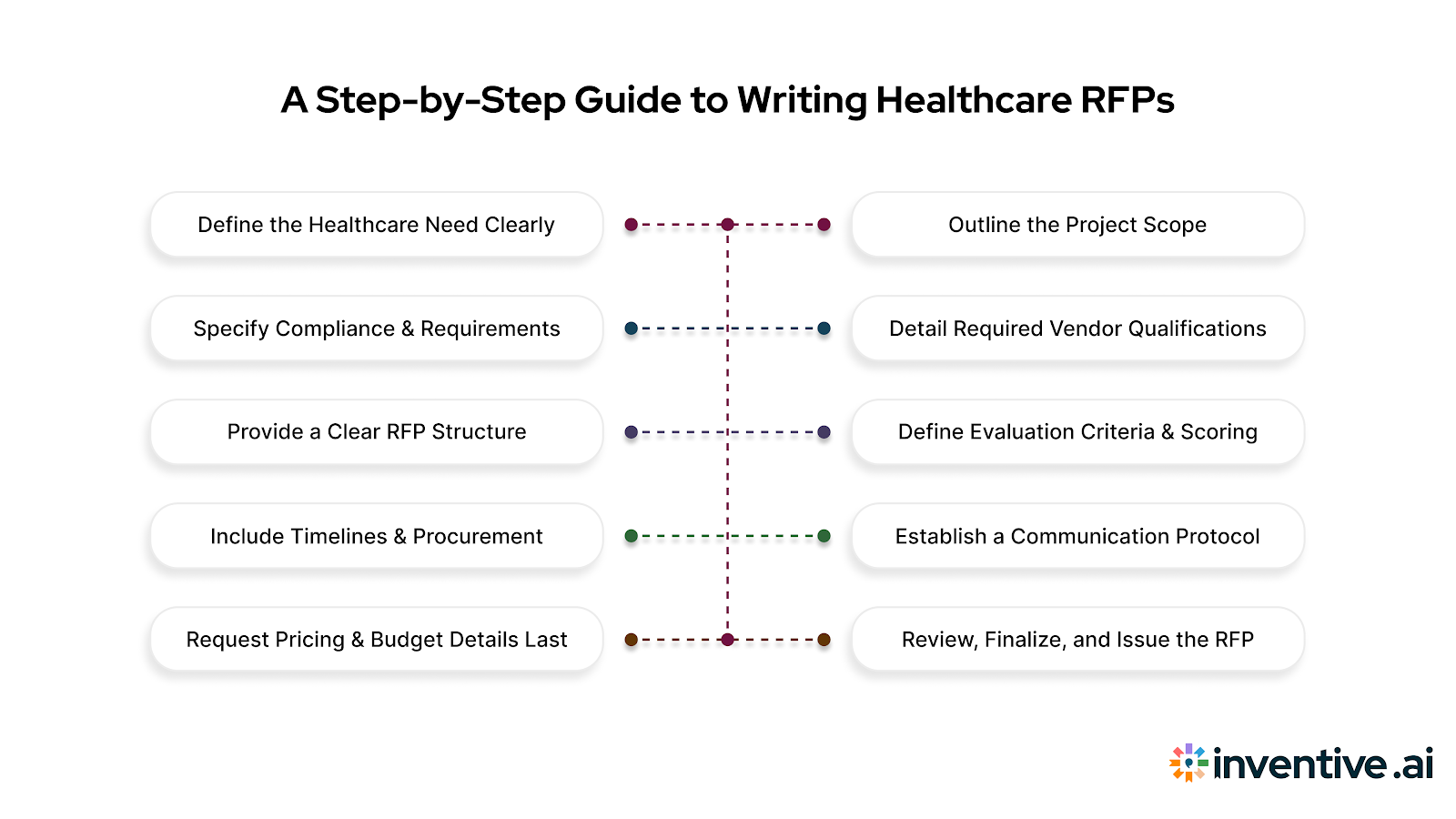
1. Define the Healthcare Need Clearly
Start by describing the clinical, operational, or technological problem your organization is trying to solve. Whether it’s implementing a new EHR system, improving patient flow, acquiring diagnostic equipment, or outsourcing clinical services, clearly articulate the need and expected outcomes. This sets the direction for the entire RFP.
2. Outline the Project Scope and Deliverables
Provide a high-level scope of work that explains what the vendor is expected to provide. In healthcare, this may include service levels, staffing requirements, equipment specifications, data integration needs, or compliance expectations. Being specific here prevents misunderstandings during implementation.
3. Specify Compliance and Regulatory Requirements
Healthcare procurement must adhere to strict legal and regulatory frameworks. Include requirements related to HIPAA, HL7/FHIR data standards, credentialing, accreditation, cybersecurity, safety protocols, or FDA/CE certifications. Compliance clarity reduces risk and filters out unqualified vendors early.
4. Detail Required Vendor Qualifications
List the experience, certifications, and capabilities a vendor must demonstrate to be considered. This can include clinical backgrounds, technical expertise, past projects in similar healthcare environments, security certifications, or evidence of high-quality patient outcomes. This ensures only capable vendors advance to the next stage.
5. Provide a Clear RFP Structure and Submission Format
Make it clear to vendors how they should organize their bids. Outline the parts they need to include: the pricing model, the technical approach, the team structure, the executive summary, and the implementation plan. It's easier and more fair to grade when the format is always the same.
6. Define Evaluation Criteria and Scoring
Share the criteria your organization will use to assess submissions. Healthcare RFPs often evaluate vendors on clinical quality, safety, interoperability, risk mitigation, cost structure, and long-term support. Transparent scoring builds trust and reduces disputes during vendor selection.
7. Include Timelines and Procurement Milestones
Publish key dates such as Q&A deadlines, submission deadlines, demonstration periods, site visits, and award timelines. Healthcare projects depend heavily on coordinated planning, so a clear timeline helps vendors allocate the right resources.
8. Establish a Communication Protocol
Identify who vendors can contact for questions and how they should submit inquiries. Restricting communication to a formal process ensures fairness, protects sensitive information, and keeps the procurement process compliant.
9. Request Pricing and Budget Details Last
Healthcare pricing is different from other fields because it often depends on a lot of different factors, such as clinical workload, consumables, software licensing, device maintenance, training, and regulatory reporting. Ask for full price breakdowns at the end of the RFP so that safety and clinical quality can be checked first.
10. Review, Finalize, and Issue the RFP
Before publishing, review the document with clinical leaders, compliance officers, IT teams, and legal counsel. Ensuring accuracy across departments helps avoid rework, ensures high-quality submissions, and leads to better vendor partnerships.
How to Write a Winning Healthcare RFP Response Using Inventive AI?
Healthcare RFP responses demand speed, precision, and airtight compliance. Inventive AI is designed specifically to handle these requirements, helping vendors produce accurate, audit-ready proposals without manual overload.
Here’s how to use Inventive AI step by step to create a winning healthcare RFP response.
1. Upload the Healthcare RFP into Inventive AI
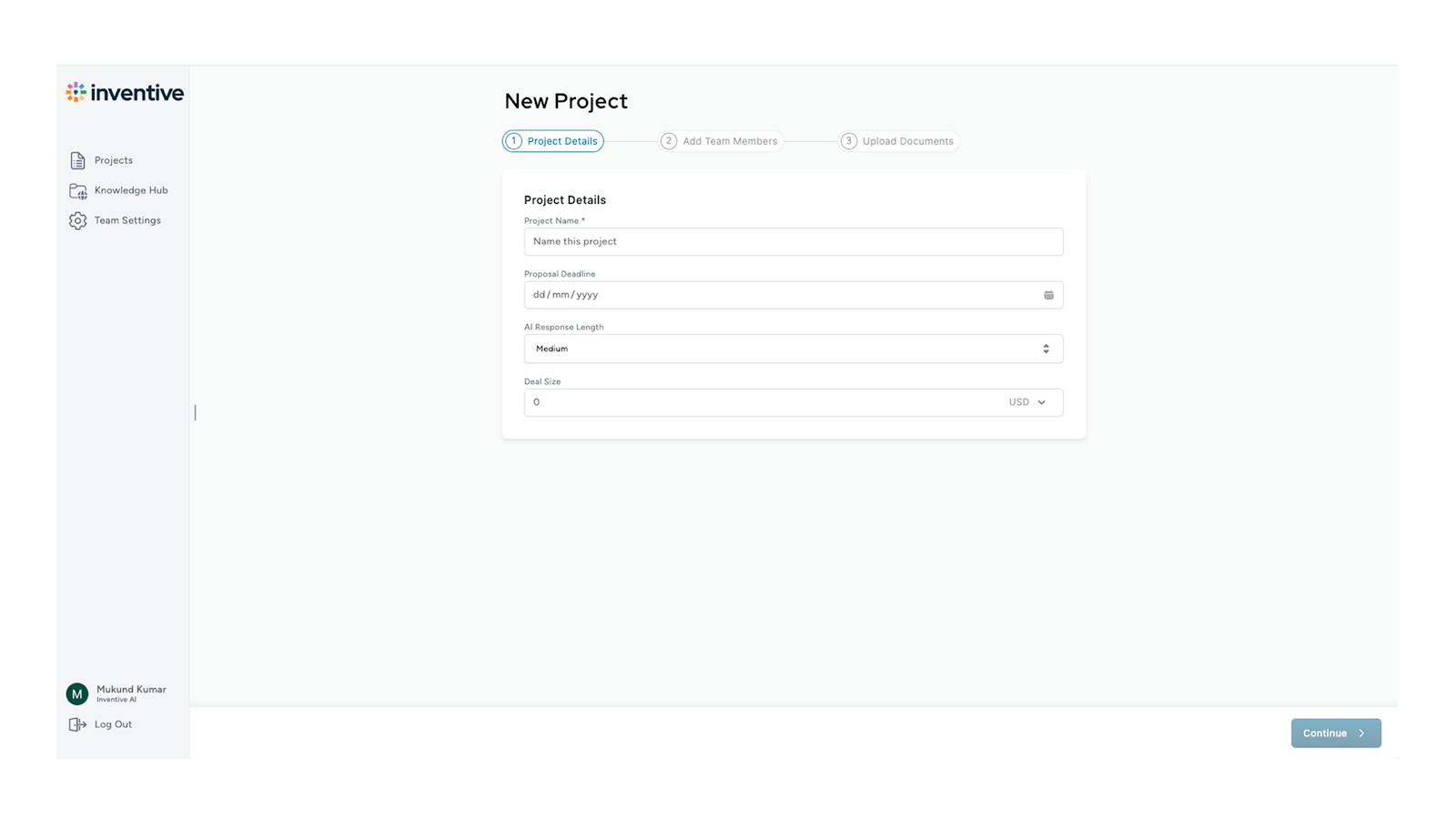
Start by uploading the full RFP document into Inventive AI. The platform automatically parses the document, identifies sections, questions, compliance requirements, and deadlines. This eliminates manual reading and ensures no clinical, technical, or regulatory requirement is missed.
2. Auto-Generate First Draft Responses from Your Knowledge Base
Inventive AI instantly generates draft responses using your approved content library, past healthcare proposals, and compliance documents.
This includes answers related to:
- HIPAA and security controls
- Technical capabilities
- Clinical workflows
- Implementation methodology
You get a complete first draft in minutes instead of days.
3. Enforce Built-In Healthcare Compliance Checks
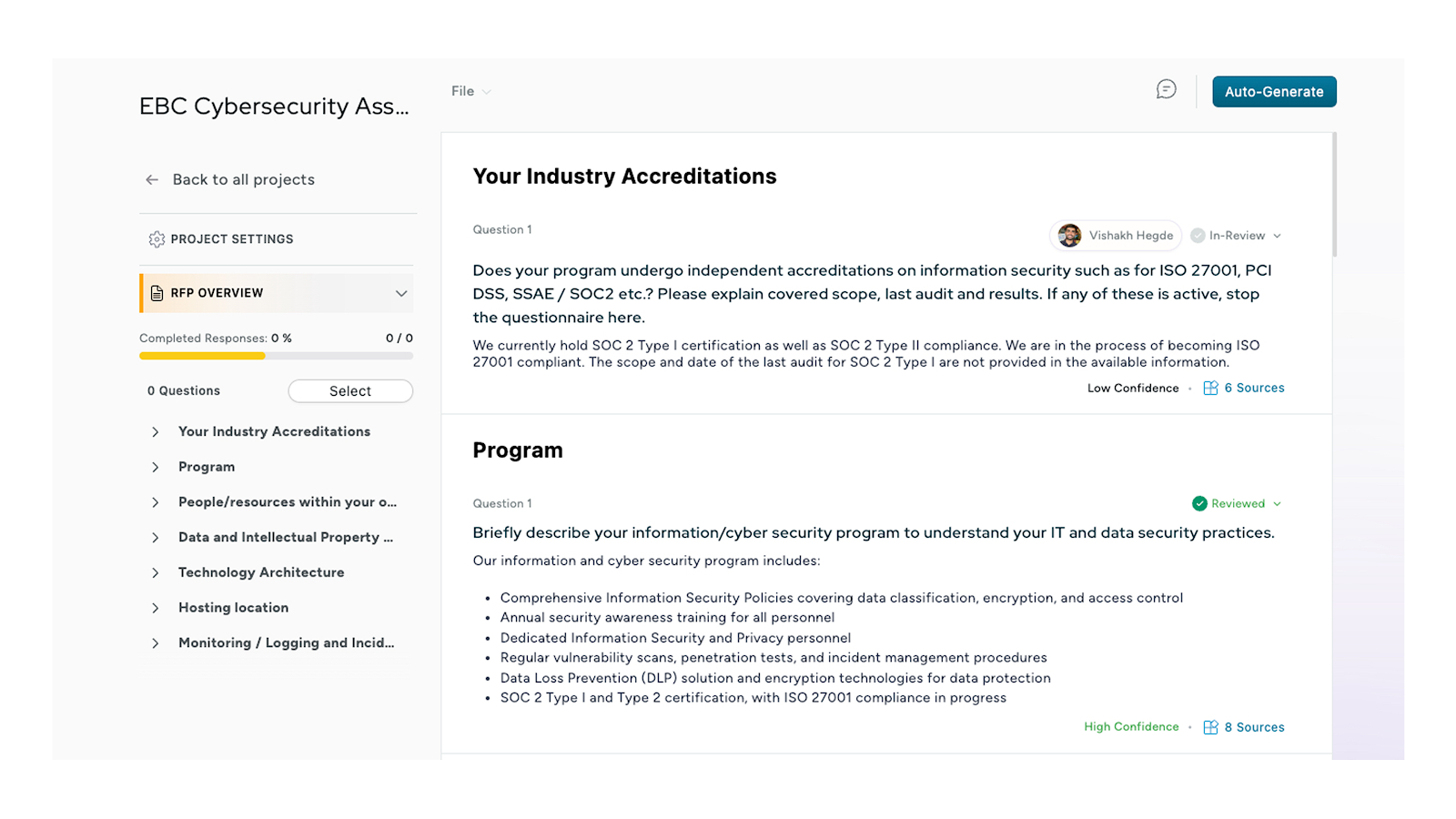
Inventive AI automatically flags missing or incomplete compliance elements such as:
- HIPAA BAAs
- Data security and PHI handling
- FDA or device certifications
- HITRUST or cybersecurity requirements
This ensures your response aligns with healthcare regulatory expectations before review even begins.
4. Customize Responses to Match the Healthcare Buyer’s Context
Use Inventive AI’s smart editing and suggestion engine to tailor responses to the specific hospital, payer, or health system.
You can quickly:
- Adjust language to match clinical or IT stakeholders
- Add patient-outcome–focused value statements
- Align terminology with the buyer’s environment
This avoids generic, copy-paste responses that often lose points during evaluation.
5. Collaborate Across Teams in One Workspace
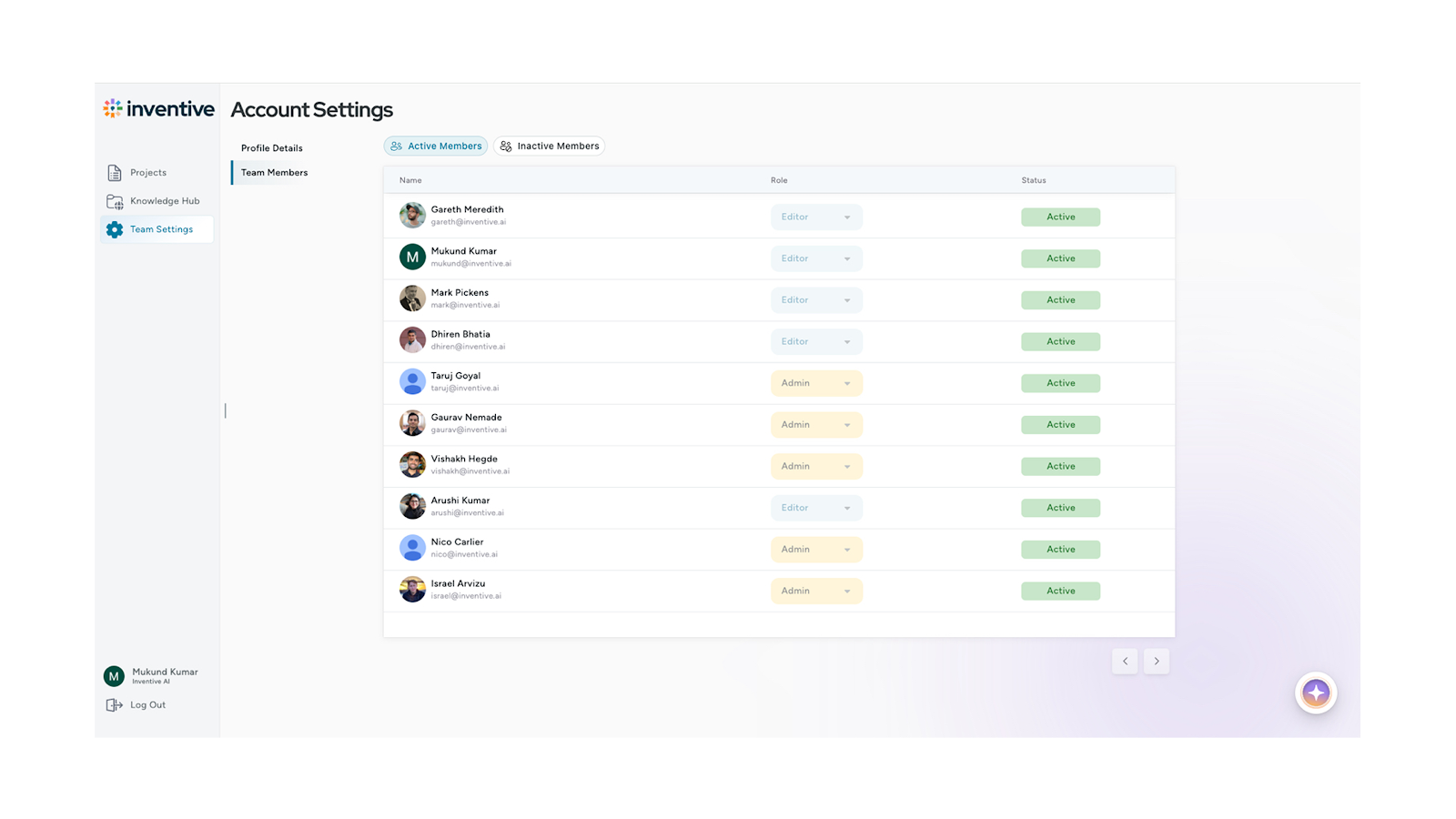
Inventive AI enables real-time collaboration between sales, clinical experts, IT, legal, and compliance teams. Each stakeholder can review, comment, and approve their sections directly inside the platform, eliminating email chains and version confusion.
6. Use AI-Powered Review to Reduce Errors Before Submission
Before finalizing, Inventive AI runs automated quality checks to:
- Detect unanswered or weak responses.
- Highlight inconsistencies across sections.
- Ensure formatting and structure match the RFP exactly.
This reduces the risk of rejection due to missing details or formatting issues.
7. Generate Final, Submission-Ready Proposal Instantly
Once approved, Inventive AI compiles the complete healthcare RFP response into a clean, submission-ready format aligned with buyer instructions. You can export confidently, knowing the proposal is compliant, complete, and easy for evaluators to score.
8. Track Performance and Improve Future RFPs
Inventive AI captures response data, turnaround times, and win-loss insights. Over time, this helps your team:
- Identify high-performing answers.
- Improve proposal quality continuously.
- Reduce response cycles with every submission.
Key Differences in the Healthcare RFI vs. RFP
If you're bidding for healthcare contracts or managing procurement, it's vital to understand how RFIs and RFPs work together. Both play essential roles in a multi-stage procurement strategy. Knowing when to use each can save time, improve proposal quality, and meet healthcare compliance demands.
Let's break down these differences and how they fit into your process.
Purpose
An RFI (Request for Information) helps healthcare organizations gather general details about the market. It's useful when decision-makers need a sense of available solutions, vendor capabilities, and approximate pricing ranges.
An RFP (Request for Proposal) takes things further. It's a structured request asking vendors to submit competitive, detailed bids. If you're responding to an RFP, it's a formal opportunity to win business based on a client's specific criteria.
Understanding what is RFP in healthcare includes knowing it's not a casual inquiry — it's a structured, binding request.
Procurement Stage
An RFI belongs to the early discovery stage of a project. Procurement teams use it to collect background information and narrow down potential vendors.
The RFP moves into the final selection stage. At this point, healthcare organizations have a defined need, set criteria, and are ready to evaluate and choose a vendor.
If a hospital's IT team is considering new imaging software but hasn't finalized requirements, they might issue an RFI. Once those needs are precise, they'll request formal proposals through an RFP.
Detailing Level
RFIs focus on high-level, exploratory information. Vendors provide general capabilities, product overviews, or service options. You aren't expected to submit pricing or contractual details.
RFPs demand in-depth, technical, and contractual details. Healthcare organisations will ask for compliance certifications, integration capabilities, implementation timelines, and pricing models.
Before responding to a healthcare RFP, understand that it requires a significant commitment to prepare detailed technical, financial, and compliance information.
Vendor Response
Vendor responses to an RFI are optional and informal. You can decide whether to respond and how much detail to include.
In contrast, RFP responses are formal and binding in nature. You're expected to meet submission deadlines and deliver complete, accurate proposals. Procurement teams use your RFP submission as an official record during evaluations and contract negotiations.
Missing a requirement or deadline in an RFP can disqualify your proposal, a risk you can't afford in regulated healthcare environments.
When to Use an RFI vs. an RFP in Healthcare Procurement?
Healthcare procurement teams typically use an RFI to research the market, gather options, and define project needs.
An RFP follows once project details, budgets, and decision-makers are in place. This sequence ensures proposals are requested only when teams are ready to act.
For vendors, participating in an RFI can position you for future RFP invitations. It's a chance to introduce your solutions and build awareness early.
Both RFIs and RFPs are essential parts of a structured procurement strategy. They help healthcare systems manage risk, meet compliance, and select vendors efficiently.
Now that we've covered how RFIs and RFPs differ, let's address the specific challenges traditional healthcare procurement teams and vendors face and how AI can improve that process.
Top 6 Common Challenges in Traditional Healthcare RFP/RFI Processes
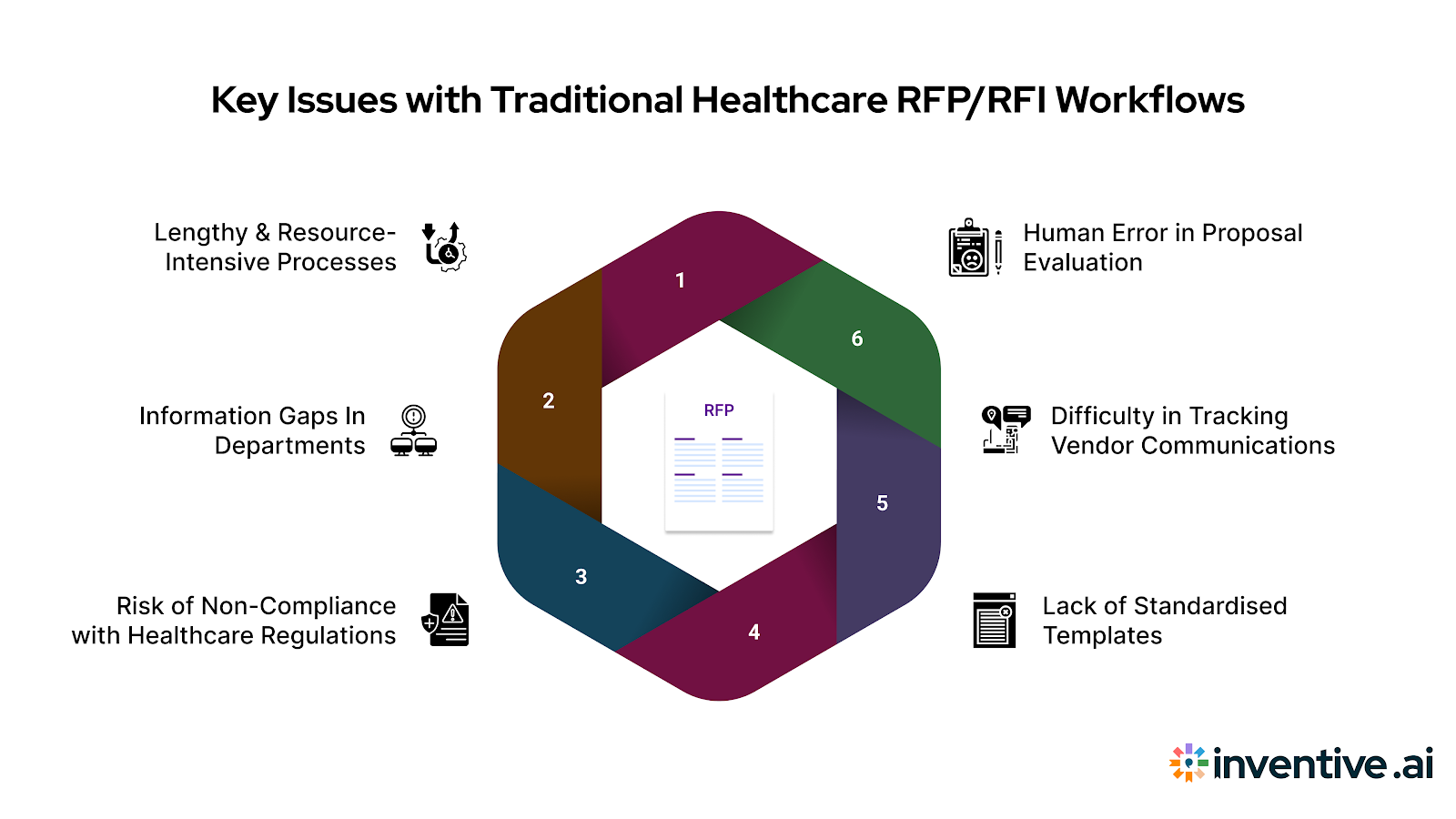
If you work in healthcare procurement or respond to bids, you've likely experienced how complex these processes can get.
Traditional RFI and RFP workflows often slow decision-making and create operational risks despite their value.
Understanding these challenges is key to improving how you handle what is RFP in healthcare today.
Let's look at healthcare teams and vendors' most common pain points.
1. Lengthy and Resource-Intensive Processes
Traditional RFPs and RFIs demand time, staff, and endless document management. Healthcare organizations often spend weeks gathering requirements, reviewing vendor proposals, and ensuring compliance checks.
For vendors, this means delayed decisions and increased proposal costs. A 2024 HIMSS survey found that 68% of healthcare providers manage procurement manually. It’s a costly inefficiency that both sides feel.
2. Information Gaps In Departments and Inconsistent Documentation
Procurement rarely happens in a vacuum. Clinical, IT, legal, and finance teams must weigh in. Unfortunately, these groups often work in silos. Each department tracks vendor details differently, creating gaps and duplicated work.
For vendors, understanding what is RFP in healthcare also means recognising that miscommunication within a health system can lead to incomplete or inconsistent proposals, impacting your chances of selection.
3. Risk of Non-Compliance with Healthcare Regulations
Healthcare procurement demands strict compliance. Every proposal must align with regulations like HIPAA, FDA guidelines, and HITRUST standards. Without a centralised, compliant process, teams risk missing critical checks.
Vendors who overlook regulatory details in RFP responses may face immediate disqualification. That’s why thorough, regulation-aligned documentation is non-negotiable in healthcare RFPs.
4. Lack of Standardised Templates
Many hospitals lack consistent RFP and RFI templates. Each department may create its own format, structure, and submission rules. This inconsistency makes it harder for vendors to submit complete, compliant, comparable proposals.
It also slows down evaluation because procurement teams can’t easily compare responses side by side. Understanding what is RFP in healthcare includes knowing when to start with an RFI and expecting varied document structures; both tools work together to create a smooth, accountable vendor selection process that requires readiness to adapt.
5. Difficulty in Tracking Vendor Communications and Responses
Healthcare procurement often involves dozens of vendors, each sending questions, attachments, and clarifications. Managing this through email or spreadsheets creates confusion. Deadlines get missed, documents go untracked, and decision cycles drag.
For vendors, poor communication tracking means updates or clarifications might not reach every participant equally, putting your proposal at risk.
6. Human Error in Proposal Evaluation
Manual scoring and evaluation of RFP responses leave too much room for error. Biases, missed criteria, or inconsistent scoring can impact fair vendor selection. Even minor mistakes in healthcare procurement can lead to costly project delays or regulatory penalties.
Understanding what is RFP in healthcare includes recognising that without proper tools, subjective and error-prone evaluation processes may negatively affect your proposal’s success.
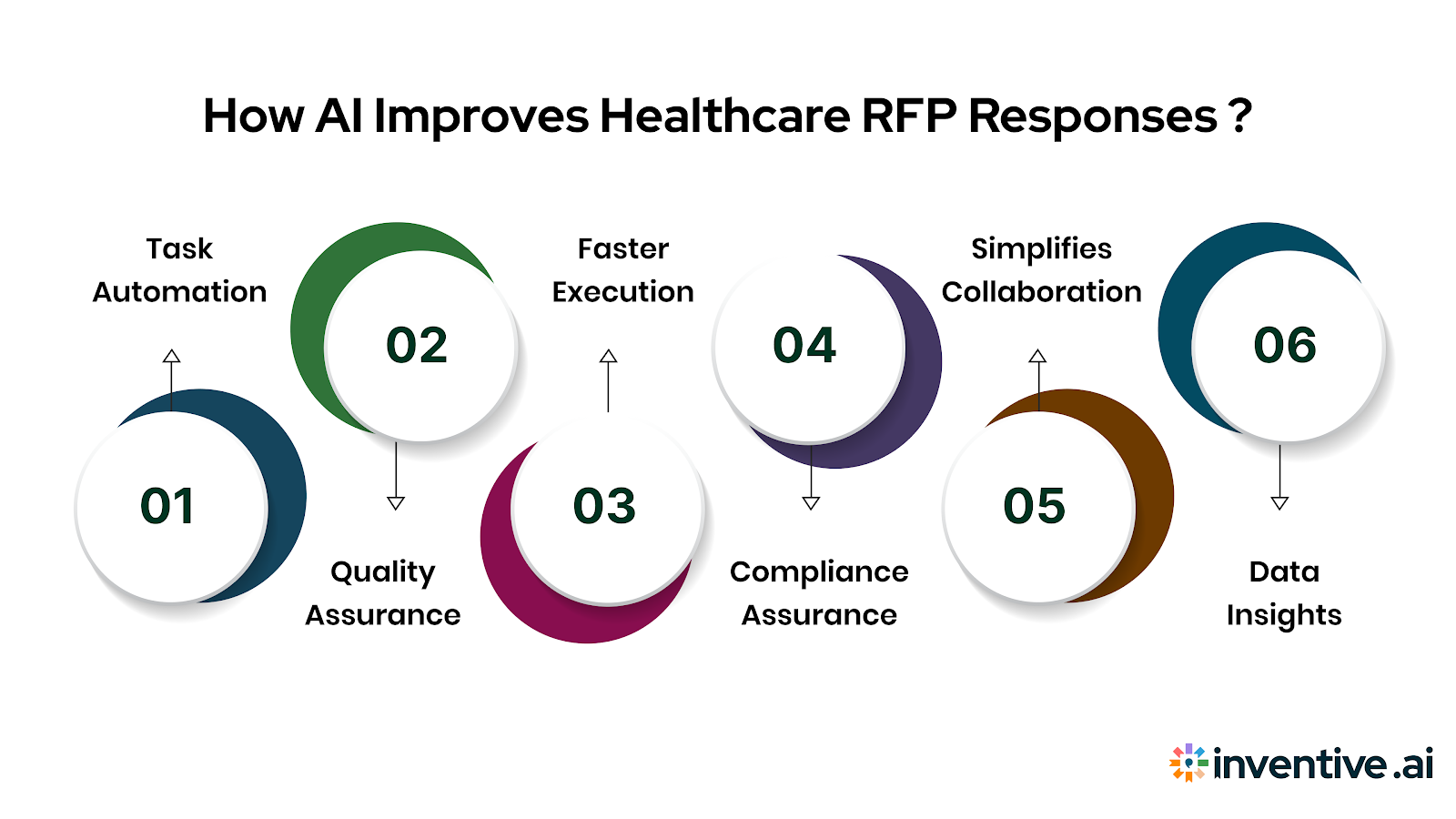
How AI Improves RFP Responses in Healthcare?
Responding to healthcare RFPs isn't simple. You deal with strict deadlines, complex compliance checks, and varied submission formats. Without the right tools, it's easy to waste time or miss critical details. That's where AI makes a measurable difference.
AI-driven RFP software enables healthcare vendors to respond faster, more accurately, and with greater alignment to client needs. If you’ve been wondering what is RFP in healthcare and how to handle them efficiently, AI is now central to that conversation.
Here are the key ways to transform AI response management:
1. Automates Repetitive Tasks
AI removes hours of manual copy-paste work. It auto-populates RFP responses using a vetted, centralized knowledge base. That means faster, consistent answers for common compliance, pricing, and capability questions. Nearly half of routine office and administrative tasks (about 46%) are ripe for automation. That’s why RFP process automation isn’t an optional upgrade; it’s essential.
2. Improves Response Quality and Consistency
By analyzing previous high-performing proposals, AI suggests the best-fit answers for each question. This raises the overall quality of your submissions and ensures every response aligns with client expectations.
3. Speeds Up Turnaround Times
RFP cycles in healthcare are notoriously slow. AI tools cut those timelines by generating first drafts in minutes, not hours. Vendors can focus on customizing strategic sections rather than wrestling with template formatting.
4. Reduces Risk of Compliance Errors
AI-powered checks flag incomplete, non-compliant, or inconsistent responses before submission. In regulated healthcare environments, this is critical to avoid costly mistakes.
5. Simplifies Collaboration
AI tools allow real-time, cloud-based collaboration. Legal, IT, clinical, and procurement teams can review, comment, and approve proposals in one workspace, eliminating back-and-forth email chains.
6. Enables Data-Driven Decision Making
Built-in analytics track response times, win rates, and content performance. Over time, vendors can see which answers resonate and adjust their strategy.
AI can streamline healthcare RFP responses, but it cannot offset regulatory missteps. Compliance remains the most common reason proposals fail, so understanding key pitfalls is critical.
Top Compliance Pitfalls in Healthcare RFPs (and How to Avoid Them)
In healthcare procurement, compliance isn't just a formality but a legal, financial, and operational safeguard. One missed requirement can stall a project or trigger regulatory penalties.
Yet, many vendors and procurement teams stumble over the same avoidable mistakes. Here are the most common compliance pitfalls in healthcare RFPs and how to sidestep them.
1. Incomplete HIPAA, FDA, and HITRUST Documentation
Healthcare RFPs typically demand strict adherence to privacy and product safety regulations. Missing or incomplete documentation like HIPAA Business Associate Agreements (BAAs), FDA approvals for medical devices, or HITRUST certifications for IT solutions can instantly disqualify a proposal.
Why it matters:
Regulators like the U.S. Department of Health and Human Services (HHS) impose steep fines for non-compliance, and hospitals cannot afford to engage vendors who lack verified protections for Protected Health Information (PHI).
For example, if you're proposing a telehealth platform without attaching your HIPAA BAA or security risk assessment, procurement teams may automatically reject your bid for regulatory non-compliance.
How to avoid it:
Create a centralized, up-to-date compliance document library that your proposal teams can quickly access. Before submission, cross-reference the RFP's compliance requirements with your checklist to ensure all required documents, including HIPAA BAA, FDA approvals, HITRUST, and others, are attached and current.
2. Misaligned or Generic Data Security Protocols
Healthcare RFPs often require detailed descriptions of how vendor solutions protect sensitive patient data. Generic, copy-pasted answers about data encryption, user access, and incident response won't satisfy compliance teams evaluating vendor risk.
Why it matters:
Healthcare data breaches cost an average of $10.93 million per incident in 2024. Health systems demand documented, HIPAA-compliant protocols tailored to their technical environment and specific data handling expectations.
For example, an EHR vendor submitting a boilerplate security response without addressing multi-factor authentication or integration safeguards with the hospital's existing systems risks rejection, not because the platform is insecure, but because the reaction lacked specificity.
How to avoid it:
Customize your data security narrative for each proposal. Reference the client's stated encryption standards (e.g., AES-256), describe PHI access controls, and explain how your breach detection protocols integrate with the healthcare organization's infrastructure. Align your answer to both HIPAA rules and any additional requirements called out in the RFP.
3. Ignoring Local and State Healthcare Regulations
Many healthcare vendors focus on national standards like HIPAA and FDA approvals but overlook applicable state-specific healthcare laws or licensure requirements. This oversight can cause legal and operational delays post-award.
Why it matters:
Several states have stricter privacy, telehealth, or data-sharing regulations than federal laws. If your proposal doesn't demonstrate awareness of these rules, it signals risk to procurement and legal teams.
For example, a telehealth vendor proposing services in California without addressing CCPA (California Consumer Privacy Act) or state telehealth consent rules may be flagged during evaluation.
How to avoid it:
Review the RFP carefully for any state law references. If absent, proactively research applicable local healthcare regulations for the hospital's location. Include a compliance statement confirming alignment with both federal and regional mandates, which positions your proposal as thorough and low-risk.
4. Vague Data Retention and Breach Notification Policies
Many proposals fail to clearly define how long PHI will be retained, how it's securely deleted, or how breach notifications will be handled. Ambiguous or inconsistent policies create legal liabilities for the healthcare client.
Why it matters:
Under HIPAA, vendors must notify covered entities within 60 days of a data breach. Hospitals need confidence that your incident response timelines and protocols align with this requirement and internal escalation procedures.
If your RFP response mentions "prompt breach reporting" without specifying timeframes or points of contact, procurement teams may flag your proposal for review delays or rejection.
How to avoid it:
Include a dedicated section in your RFP response outlining your data retention schedules, secure destruction protocols, and breach notification policy. Be explicit: state exact timeframes (e.g., "Data retained for 7 years in compliance with HIPAA and securely purged thereafter") and notification windows.
5. Missing Accessible Patient Data Handling Policies
Inadequately addressing how PHI is accessed, shared, and audited by authorized users within your solution can result in RFP rejection, especially for clinical or administrative software proposals.
Why it matters:
Hospitals must verify that vendors have strict access controls, detailed audit logs, and processes to prevent unauthorized PHI exposure. It's not enough to say data is "secure," evaluators need to know how.
For example, a patient engagement app proposal without explaining role-based access or audit trails will appear incomplete, raising doubts about compliance readiness.
How to avoid it:
In your proposal, outline access controls in detail:
- Define who can access what data
- Describe how access is granted and revoked
- Explain how access attempts and actions are logged and audited
Provide examples or diagrams if appropriate, ensuring your explanation is both HIPAA-compliant and tailored to the healthcare client's operational structure.
By anticipating these pitfalls and proactively addressing them in your proposals, you not only protect your bid from disqualification but also position your organization as a responsible, risk-aware partner.
We hope you now have a better idea about RFIs and RFPs in healthcare procurement. Now, let's explore how Inventive AI helps healthcare teams and vendors solve these challenges with faster, wiser, and more compliant RFI and RFP management.
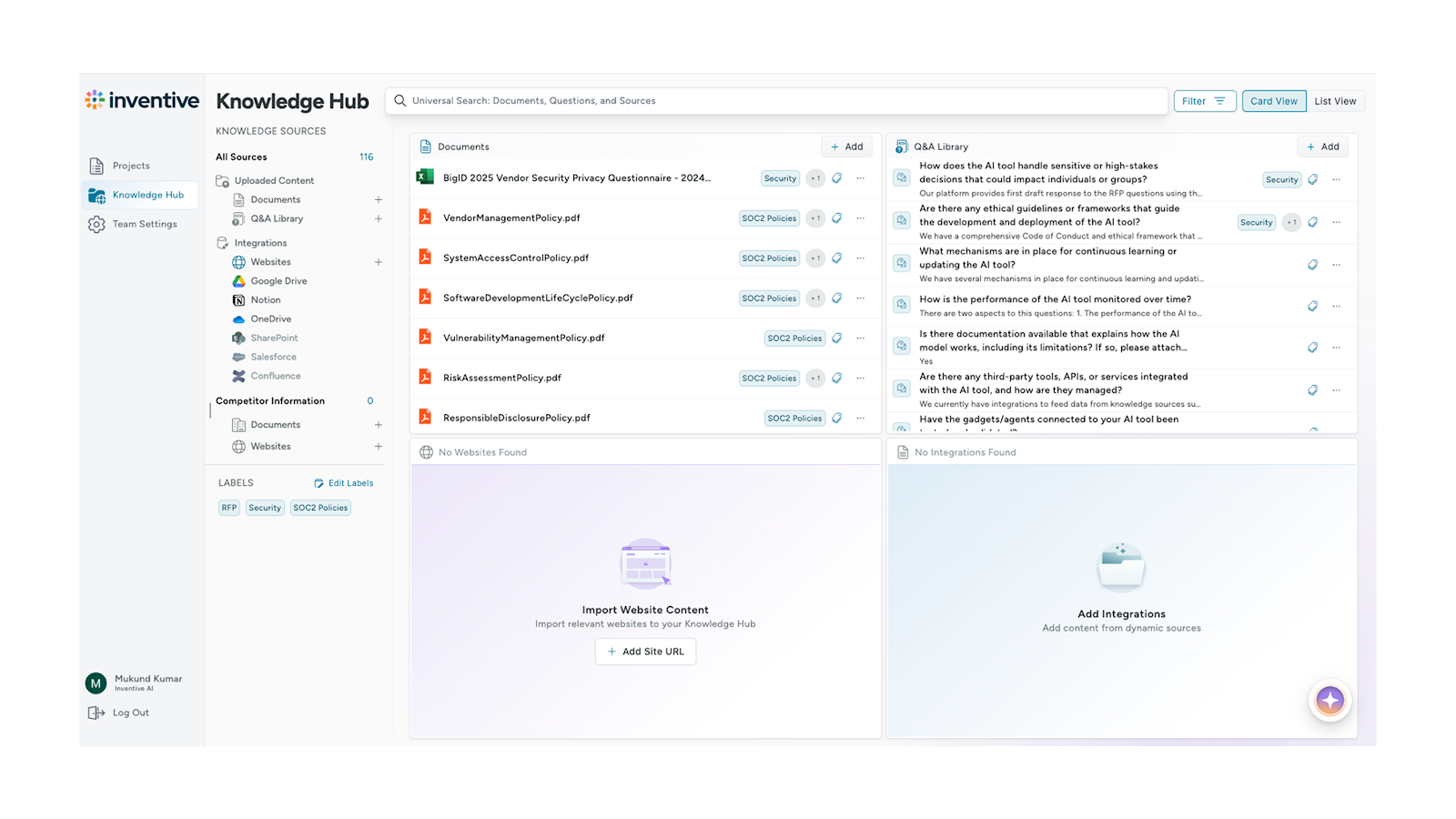
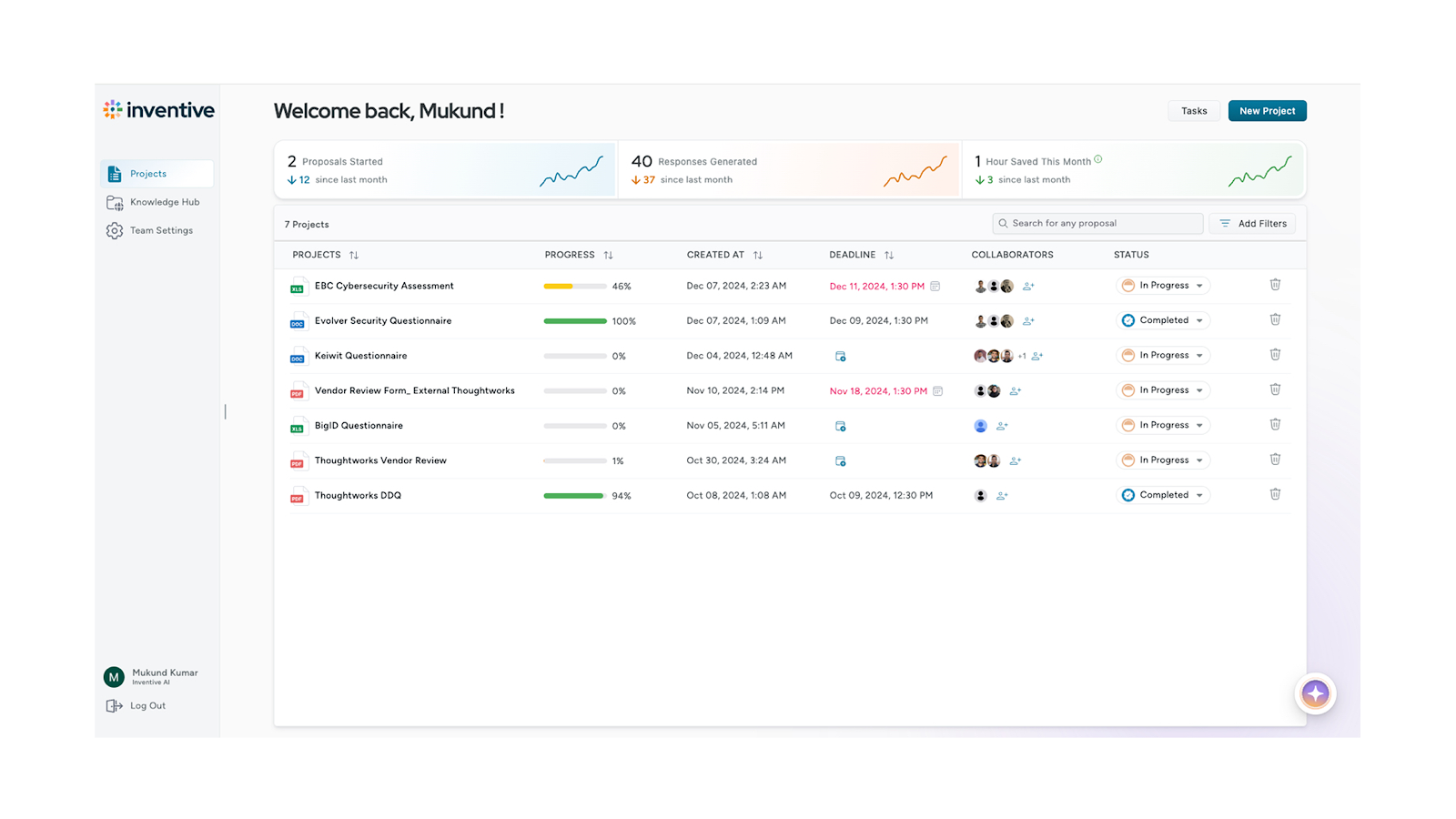
How Inventive AI Transforms RFI/RFP in Healthcare?
Inventive AI is purpose-built to simplify complex, high-stakes procurement processes in healthcare. It helps procurement teams and vendors work faster, stay compliant, and improve decision quality. With AI-driven automation, hospitals reduce RFP cycle times by up to 70% and cut manual workloads by over 60%.
If you work with what is RFP in healthcare processes, here's where Inventive AI makes an impact:
- Automates RFP response generation and proposal scoring for faster, consistent evaluations.
- Speeds up RFI creation using intelligent templates and historical healthcare procurement data.
- E.
- Provides collaborative workspaces for procurement, IT, clinical, and legal teams to review and approve together.
- Includes real-time analytics dashboards for proposal scoring, vendor comparisons, and cycle tracking.
- Manages version control, deadlines, and vendor communications from a single, organized platform.
See how it works for your teams →

Frequently Asked Questions (FAQs)
1. What is the difference between an RFI and an RFP in healthcare procurement?
An RFI (Request for Information) is a preliminary step used to gather broad insights about vendor capabilities or market offerings, ideal when project requirements are still evolving. An RFP (Request for Proposal), in contrast, is a formal request issued when requirements are precise and the procurement team is ready to evaluate structured proposals from potential vendors.
2. Does an RFI include pricing information?
RFIs typically do not focus on pricing and are not binding; their goal is to assess vendor suitability. Pricing is usually addressed later, such as during an RFQ (Request for Quotation) or RFP phase, once project scope and vendor shortlist are defined.
3. When should procurement teams use an RFQ versus an RFP?
Choose an RFQ when the project requirements are well-defined and price is the primary evaluation factor, common in standard, commoditized purchases. Use an RFP for more complex needs where qualitative factors like technical capability, integration, compliance, and service support matter more than price alone.
4. Why use an RFI before launching an RFP?
Issuing an RFI first helps refine your requirements, assess vendor qualifications, and avoid issuing overly broad or under-informed RFPs. It's a strategic step to build clarity and shortlist suitable vendors before asking them for detailed proposals.
5. How long does a typical healthcare RFP process take?
Healthcare RFP cycles are known to be lengthy, often ranging from six months to a few years, due to budget approvals, stakeholder alignment, regulatory compliance, and the complexity of clinical and technical requirements.
6. Can vendors assume procurement teams review every RFI/RFP response?
Yes. Responses are typically formally reviewed and scored, especially in regulated healthcare settings. While not every individual section may influence the final decision, the document as a whole will be evaluated, often using structured scoring matrices and follow-up interviews or demos.

90% Faster RFPs. 50% More Wins. Watch a 2-Minute Demo.
Understanding that sales leaders struggle to cut through the hype of generic AI, Mukund focuses on connecting enterprises with the specialized RFP automation they actually need at Inventive AI. An IIT Jodhpur graduate with 3+ years in growth marketing, he uses data-driven strategies to help teams discover the solution to their proposal headaches and scale their revenue operations.
Tired of watching deal cycles stall due to manual questionnaire back-and-forth, Dhiren co-founded Inventive AI to turn the RFP process from a bottleneck into a revenue accelerator. With a track record of scaling enterprise startups to successful acquisition, he combines strategic sales experience with AI innovation to help revenue teams close deals 10x faster.

.jpeg)
