Healthcare RFP Management: Top 10 Strategies
Simplify healthcare RFP management with centralized tools; boost collaboration with stakeholders, and set clear evaluation criteria.

Are delays and compliance hurdles slowing down your healthcare RFP approach?
Healthcare RFP management refers to the process of planning, drafting, and managing Requests for Proposals in the healthcare sector. It ensures that procurement aligns with clinical needs, regulatory requirements, and operational goals.
Yet, industry data shows RFP win rates hover at just 45%, indicating room for major performance gains. In high-stakes healthcare environments, mistakes in compliance, coordination, or clarity can compromize patient safety, increase costs, and delay critical projects. RFPs here must balance precision, urgency, and transparency to succeed.
In this guide, you will learn the top 10 strategies in healthcare RFP management, from meeting clinical standards to using technology effectively.
Key Takeaways
- RFPs in healthcare ensure structured vendor selection, compliance, and cost control.
- Strong healthcare RFP management reduces risks linked to accuracy, timelines, and regulatory standards.
- Clear strategies like collaboration, detailed evaluation, and structured templates improve outcomes.
- Considering factors such as budget, compliance, and vendor expertize leads to better decisions.
- Avoiding common mistakes like vague requirements or poor timelines strengthens the RFP process.
Importance of RFPs in Healthcare Management
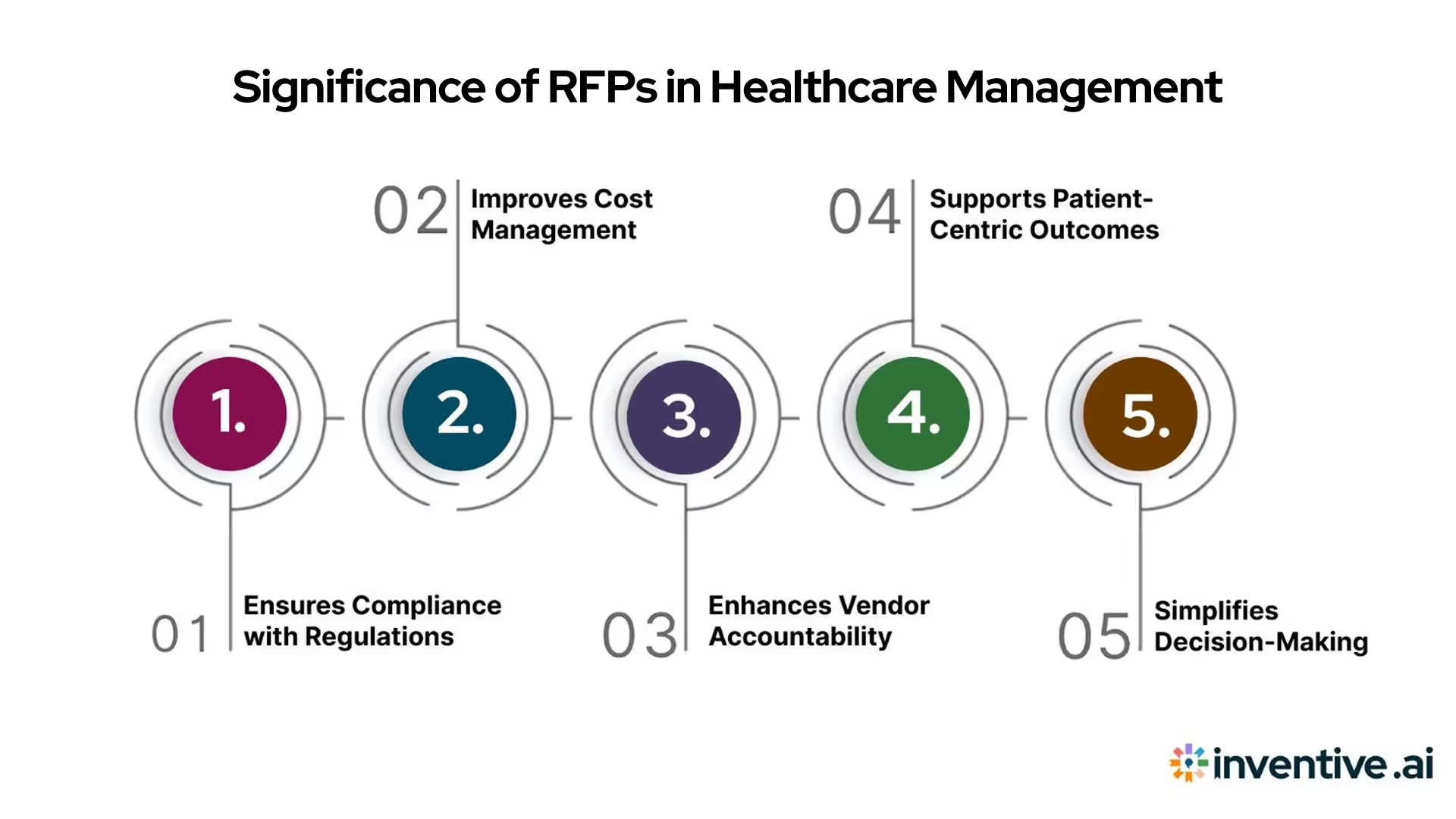
RFPs in healthcare serve as a structured way to source products, services, and technology while ensuring compliance with strict standards. They enable fair vendor evaluation and help align procurement with clinical and operational priorities. Done well, they improve efficiency, reduce risks, and support better patient care outcomes.
These five points outline why RFPs hold such an important role in healthcare procurement.
- Ensures Compliance with Regulations
Healthcare procurement involves strict oversight from bodies like the FDA, HIPAA, and CMS. A healthcare RFP management process ensures vendors meet these regulations before contracts are awarded. It reduces the risk of penalties, protects patient data, and maintains trust between providers and their communities.
- Improves Cost Management
RFPs allow side-by-side comparisons of pricing, terms, and deliverables. This transparency helps decision-makers select options that provide long-term value. In a field where budgets are tight, this structured evaluation reduces unnecessary spending without compromizing on quality.
- Enhances Vendor Accountability
Clear requirements and scoring criteria hold vendors accountable from the start. It reduces disputes during implementation, as expectations are set early. Vendors who understand the healthcare sector’s demands are more likely to deliver on time and within budget.
- Supports Patient-Centric Outcomes
RFPs help align purchases with patient needs by ensuring proposed solutions improve care delivery. Whether acquiring diagnostic tools or patient management systems, this focus ensures resources directly benefit health outcomes rather than only operational convenience.
- Simplifies Decision-Making
A structured RFP process removes ambiguity by defining evaluation metrics and timelines upfront. It speeds up approvals, avoids unnecessary back-and-forth, and ensures procurement teams and clinical leaders work from the same set of facts.
When structured correctly, healthcare RFP management reduces risks, optimizes costs, and improves care delivery. Now, let’s discuss the steps for an effective healthcare RFP management.
A Step-by-Step Guide for Healthcare RFP Management
Effective healthcare RFP management requires a deliberate process that balances strict compliance, technology requirements, budget transparency, and patient outcomes. Following a structured approach helps healthcare organizations avoid common pitfalls and secure the best-fit solutions for clinical and operational needs.
Here are 7 essential steps for managing healthcare RFPs from start to finish:
1. Define Needs and Stakeholder Requirements
Begin by gathering input from clinical teams, IT, procurement, and leadership to outline objectives, constraints, and measurable outcomes. It ensures the RFP addresses both operational and patient-facing needs from the outset.
2. Draft Precise RFP Documents
Clearly define technical and functional requirements, scope of services, compliance expectations (e.g., HIPAA, FDA), and evaluation criteria. Include detailed project goals, deliverables, qualification standards, and submission guidelines to set vendor expectations.
3. Conduct Market Research and Vendor Shortlisting
Survey the market for technology and service trends, benchmark peer organizations, and build a longlist of qualified vendors. Use project needs and compliance factors to create a focused shortlist and invite the best candidates.
4. Release RFP and Manage Q&A
Issue the RFP to shortlisted vendors, set clear submission deadlines, and provide a structured Q&A period. Address all vendor queries promptly to clarify requirements and eliminate complexities, supporting fair and accurate proposals.
5. Evaluate Proposals Against Set Criteria
Score each response using a defined rubric for compliance, cost, technical fit, vendor experience, and patient impact. Involve relevant clinical and operational stakeholders in the review process to ensure a holistic evaluation.
6. Select Vendor and Negotiate Contract
Choose the proposal that best meets priorities for compliance, value, and operational readiness. Negotiate contract terms to address implementation timelines, SLA commitments, pricing, training, and risk mitigation.
7. Plan Implementation and Training
Collaborate with the selected vendor on deployment planning, integration with existing systems, and a comprehensive training schedule. Establish clear communication channels for user support and post-launch evaluations to ensure ongoing success.
Also Read our informative guide on RFP in Healthcare Procurement.
A disciplined, step-by-step RFP management process allows healthcare organizations to maximize competition, minimize risks, and deliver high-value outcomes, all while maintaining regulatory compliance.
Next, you will learn about the proven strategies for improving the effectiveness of healthcare RFPs and achieving superior results in challenging procurement environments.
Top 10 Strategies for Successful Healthcare RFP Management

Healthcare RFP management is complex due to strict compliance rules, high stakes, and multiple decision-makers. Without a clear strategy, procurement delays and vendor mismatches can cost both time and money. By adopting the right strategies, organizations can reduce risks and achieve better outcomes.
These ten strategies highlight how to approach healthcare RFP management in a structured and results-driven way.
1. Prioritize Regulatory Compliance from the Start
Healthcare procurement must always begin with compliance. Federal and state regulations, HIPAA standards, and FDA requirements should be non-negotiable.
For example, when evaluating electronic health record systems, HIPAA compliance must be mandatory. Building compliance criteria into RFP requirements ensures only qualified vendors move forward.
This approach prevents regulatory setbacks, reduces liability risks, and builds trust with patients and stakeholders. Clear documentation of compliance also strengthens audit readiness, which is often necessary for federal reimbursements.
2. Define Clear and Measurable Evaluation Criteria
Ambiguous criteria often lead to misaligned vendor selection. Healthcare RFP management works best when scoring metrics are defined early. It could include cost, implementation time, support quality, and technical capabilities.
For instance, when procuring telehealth software, assigning specific weightage to factors like uptime, integration with existing systems, and scalability ensures objective scoring. A structured approach saves time, prevents disputes, and results in a solution that aligns with both operational and clinical priorities.
3. Align Procurement Goals with Patient Outcomes
Procurement decisions should not focus only on cost or speed but also on patient impact. For example, selecting advanced imaging equipment may come with higher upfront costs, but improved diagnostic accuracy supports better long-term outcomes.
By aligning RFP goals with clinical priorities, organizations ensure that resources support their mission of improving care quality. This alignment also helps in gaining buy-in from clinical teams, reducing resistance during implementation.
4. Build Strong Collaboration Between Departments
RFPs often stall when clinical staff, IT teams, and procurement officers work in parts. Creating a cross-functional committee avoids miscommunication.
For instance, when procuring a patient management system, IT can focus on system integration, while clinicians ensure usability. Procurement then evaluates vendor credibility. This coordinated approach results in balanced decisions that meet both technical and clinical requirements. It also reduces costly revisions that occur when one department’s needs are overlooked.
5. Standardize Documentation and Templates
Healthcare RFPs often involve multiple stakeholders and large volumes of paperwork. Using standardized templates for requirements, vendor questionnaires, and scoring systems ensures consistency. For example, instead of every department creating its own RFP draft, a hospital can use a centralized template library.
It speeds up the process and reduces errors, ensures compliance language is always included, and makes vendor responses easier to compare. Standardization strengthens accountability and reduces administrative burden.
6. Focus on Vendor Experience in Healthcare
Not every vendor understands healthcare’s unique needs. Choosing experienced vendors reduces risks during implementation. For instance, a company with proven expertize in electronic health records will already understand compliance, training, and integration requirements.
Ask vendors for case studies in similar healthcare settings to help confirm their ability to deliver. This approach avoids costly delays that occur when vendors underestimate the complexity of healthcare operations.
7. Create Realistic Timelines and Milestones
Unrealistic deadlines often compromize quality. Healthcare RFP management requires time for compliance checks, vendor clarifications, and stakeholder reviews. A structured timeline with milestones for vendor Q&A, internal reviews, and scoring ensures smoother execution.
For example, setting a clear 90-day schedule for selecting a new medical equipment provider prevents rushed decisions. It allows teams to conduct proper due diligence without slowing down essential procurement.
8. Evaluate Long-Term Value, Not Just Cost
Lowest cost is not always the best option. For example, cheaper diagnostic machines may have higher maintenance costs and shorter lifespans. Evaluating long-term value, including training, warranty, scalability, and service reliability, ensures sustainability.
Healthcare organizations should request total cost of ownership (TCO) projections from vendors. This approach protects budgets from hidden costs while ensuring quality patient care is maintained over time.
9. Encourage Transparent Communication with Vendors
Open communication reduces misunderstandings and builds stronger vendor relationships. Hosting vendor Q&A sessions during the RFP process ensures clarity on requirements. For example, hospitals sourcing surgical equipment can invite vendors to present solutions before scoring begins.
This transparency helps vendors customize their proposals better while giving procurement teams clearer insights. The result is fewer disputes and faster contract negotiations.
10. Track and Review Post-Implementation Outcomes
RFP success does not end with vendor selection. Measuring vendor performance after implementation ensures accountability. For example, if a hospital procures telehealth software, key metrics like adoption rates, patient satisfaction, and downtime should be monitored.
Tracking outcomes highlights what worked well and what needs improvement in future RFP cycles. This feedback loop strengthens procurement practices and creates a continuous improvement culture.
Successful healthcare RFP management requires discipline, collaboration, and a focus on long-term value. When strategies are applied consistently, organizations achieve compliance, reduce costs, and support better patient outcomes.
A structured approach also helps avoid common setbacks. Building on these strategies, let’s consider the essential factors that shape healthcare RFP management.
Must Read: The Ultimate Guide to the Healthcare RFI
Key Factors to Consider for Effective Healthcare RFP Management
Healthcare RFPs involve more than drafting documents and collecting bids. They demand careful consideration of multiple factors that directly affect compliance, efficiency, and patient care. Ignoring these elements can result in costly errors and delays that impact both operations and outcomes.
The following five factors serve as the foundation for managing RFPs effectively and ensuring healthcare procurement delivers sustainable results.
Compliance and Legal Requirements
Healthcare operates in a tightly regulated environment where mistakes can lead to fines or loss of funding. Every RFP must reflect HIPAA, CMS, and state-specific requirements.
For instance, medical software vendors must prove adherence to HIPAA privacy rules. Including compliance as a mandatory criterion reduces risks and strengthens audit readiness.
Budget and Financial Constraints
Cost pressures are constant in healthcare, especially for non-profit hospitals and public providers. RFPs must balance affordability with long-term value. Factoring in hidden costs like training, maintenance, and system upgrades ensures realistic budgeting.
A total cost of ownership approach helps prevent overspending while safeguarding quality care standards.
Vendor Reputation and Experience
Not all vendors understand the complexities of healthcare. Evaluating a vendor’s past performance, case studies, and industry certifications provides confidence in their ability to deliver.
For example, a vendor that has successfully implemented electronic health records in similar hospital systems is less likely to struggle with integration challenges.
Technology Compatibility and Scalability
Healthcare facilities often use interconnected systems for patient data, billing, and diagnostics. Any new solution must integrate smoothly with existing infrastructure.
Scalability is equally important, especially with the growth of telemedicine and digital health tools. RFPs should ask vendors for compatibility guarantees and future-ready technology roadmaps to avoid obsolescence.
Stakeholder Engagement and Alignment
RFPs often fail when key decision-makers are not involved. Procurement teams must engage clinicians, IT staff, and administrators early in the process. Their input ensures the chosen vendor meets operational needs and patient-focused priorities.
Strong alignment prevents delays during implementation and promotes organization-wide acceptance of new solutions.
Considering these factors ensures healthcare RFP management is thorough, cost-effective, and aligned with clinical goals. Each decision directly impacts compliance, budgets, and care delivery.
By recognizing these elements, organizations reduce risks and improve procurement outcomes. With these foundations in place, it’s equally important to understand the common mistakes that can hinder success.
Common RFP Mistakes in Healthcare Sectors
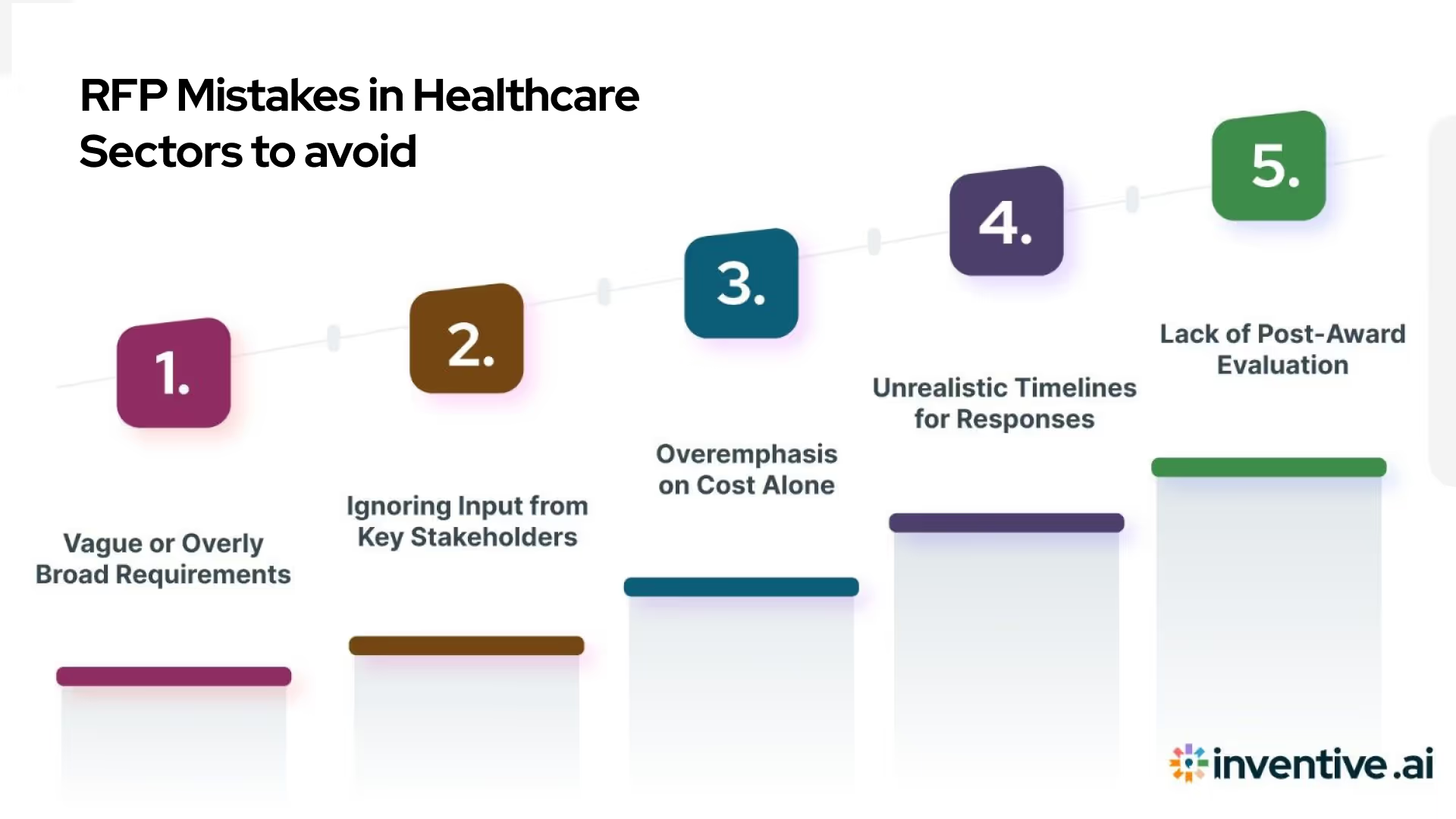
Healthcare RFPs demand precision, but many organizations still fall into recurring traps that delay results and weaken vendor selection. These mistakes are not just minor setbacks; they can compromize compliance, increase costs, and reduce service quality.
Here are 5 common errors in healthcare RFP management and practical ways to avoid them:
Vague or Overly Broad Requirements
When requirements are unclear, vendors struggle to provide accurate responses. It often results in proposals that don’t meet actual needs. For example, asking for “EHR integration” without specifying standards leaves room for misalignment.
To avoid this, detail functionality, compliance needs, and measurable outcomes so vendors can respond effectively.
Ignoring Input from Key Stakeholders
Leaving clinicians, IT staff, or finance teams out of the process can cause misaligned vendor selection. For instance, a system chosen without clinician feedback may disrupt workflows.
The solution is to involve cross-functional stakeholders early. Their input ensures that the final choice meets both technical and clinical expectations.
Overemphasis on Cost Alone
Selecting vendors solely on the lowest price is risky. While budget matters, cutting costs often compromizes quality, long-term support, and compliance. A hospital choosing the cheapest telehealth platform may later face poor data security.
To avoid this, evaluate proposals on value, scalability, and compliance, not just price points.
Unrealistic Timelines for Responses
Healthcare RFPs involve detailed compliance and technical checks. Expecting vendors to respond quickly often results in incomplete or inaccurate submissions. It creates delays later in evaluation.
To overcome this, set realistic timelines, communicate deadlines clearly, and allow time for clarifications. A structured schedule promotes accurate, competitive proposals.
Lack of Post-Award Evaluation
Many organizations end RFP management at contract signing. Without tracking vendor performance, issues may go unnoticed until they disrupt operations. For example, a delayed software rollout could have been flagged earlier with proper monitoring.
Building a post-award review process ensures vendors remain accountable and performance stays aligned with goals.
Avoiding these mistakes strengthens healthcare RFP management and saves time, money, and resources. By setting clear requirements, involving the right stakeholders, and maintaining post-award checks, organizations build stronger vendor relationships.
Also consider reading our valuable guide on Go/No-Go Decision Process: Steps & Checklist for Projects
Having addressed common errors, it’s worth examining how technology, especially AI, can improve accuracy and speed in RFP management.
AI’s Role in Healthcare RFP Management
Managing healthcare RFPs often requires sifting through hundreds of requirements, compliance checks, and vendor details. Manual methods slow the process and leave room for human error. AI adds efficiency by automating repetitive tasks and offering insights that improve accuracy in vendor selection.
Here are 5 ways AI supports healthcare RFP management effectively.
Automating Compliance Checks
Healthcare RFPs must meet strict standards such as HIPAA and HITECH. Manually verifying these requirements is time-consuming and prone to oversight. AI tools can scan proposals against compliance frameworks and flag gaps instantly. It reduces review time while ensuring that only fully compliant vendors advance in evaluation.
Smarter Vendor Matching
AI algorithms can analyze vendor databases and match proposals with organizational needs. For example, if a hospital needs a cloud-based EHR with HL7 integration, AI can quickly identify vendors meeting those criteria. It eliminates guesswork and helps decision-makers focus on qualified, relevant partners from the start.
Enhanced Data Analysis for Evaluation
Evaluating multiple proposals often involves comparing cost, service levels, and technical capabilities. AI can generate side-by-side comparisons, highlight anomalies, and even predict long-term vendor performance based on past contracts. It gives decision-makers a data-backed view, reducing bias and improving the quality of final selections.
Speeding Up Proposal Reviews
Lengthy proposals can frustrate procurement teams. AI-powered summarization tools extract key points such as pricing, timelines, and compliance details. It enables teams to review proposals faster without missing critical information. Hospitals can move from initial review to shortlisting vendors in days instead of weeks.
Predictive Insights for Better Outcomes
AI can forecast potential risks, delays, or hidden costs by analyzing proposal data and historical trends. For instance, if a vendor has a track record of delayed deliveries, AI will flag it early. These predictive insights allow organizations to negotiate better terms and avoid future disruptions.
AI transforms healthcare RFP management by making processes faster, more accurate, and less resource-intensive. From compliance checks to predictive insights, it equips decision-makers with tools for smarter choices.
Must Read: 10 Essential Steps for a Winning Vendor Selection
With these benefits in mind, it’s worth highlighting how Inventive AI brings these advantages into one practical, healthcare-focused solution.
How Inventive AI Can Help Vendors With Healthcare RFP Management?
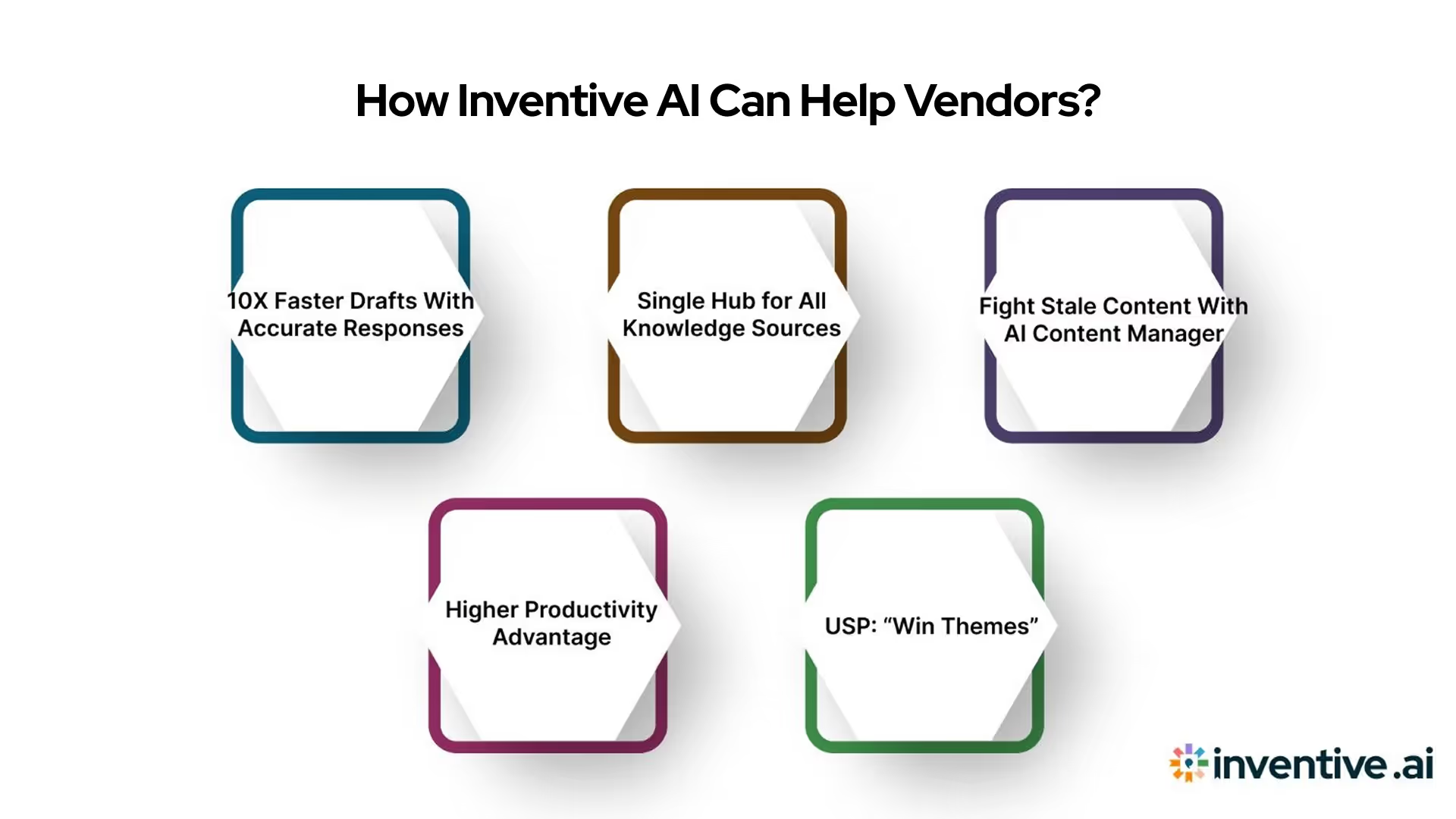
Inventive AI is a specialized platform built to simplify and strengthen RFP response management. Designed for vendors in healthcare and other complex industries, it helps teams accelerate proposal creation, centralize information, and maintain accuracy across responses. By reducing manual effort, it ensures faster, smarter, and more compliant RFP handling.
Here’s how Inventive AI’s products support vendors in managing healthcare RFP management:
- 10X Faster Drafts With Highly Accurate Responses
Our proprietary AI system delivers first drafts up to ten times faster. Responses are rooted in your verified knowledge sources, reducing errors and saving valuable time. Teams can then collaborate on these drafts, ensuring they are refined, accurate, and tailored to each proposal.
- Single Hub for All Your Knowledge Sources
Inventive AI offers a central hub for your entire knowledge base. Vendors can upload past RFPs, integrate with systems like Google Drive and SharePoint, or pull Q&A from spreadsheets and legacy tools. Even web-based content can be included, creating a single, accessible repository for accurate responses.
- Fight Stale Content With AI Content Manager
Outdated content weakens responses. Our content manager identifies conflicting or stale information within your sources, ensuring only fresh, relevant data is used. It keeps your proposals up to date and aligned with current healthcare requirements.
- Higher Productivity & Competitive Advantage
Inventive equips vendors with AI agents designed to improve research, idea generation, and competitor analysis. By automating these areas it boosts productivity, reduces time spent on manual tasks, and gives vendors a strategic edge in winning complex healthcare contracts.
- USP: “Win Themes”
Traditional RFP processes often miss key client requirements. Inventive AI’s Win Themes solve this by detecting content gaps and gathering missing details from platforms like Slack, email, and call notes. It ensures proposals are complete, client-focused, and have the strongest chance of conversion.
Conclusion
Healthcare RFP management shapes how providers, payers, and vendors collaborate to deliver quality services. They bring structure to vendor selection and compliance, ensuring decisions are transparent and data-driven. However, challenges such as strict regulatory requirements, tight timelines, and the need for absolute accuracy make RFPs complex and resource-heavy.
Successful RFP management depends on applying the right strategies: clear scope definition, stakeholder alignment, accurate compliance checks, and efficient evaluation processes. At the same time, pitfalls like vague requirements or outdated content can derail outcomes. Balancing speed with precision remains a constant challenge for healthcare organizations.
Inventive AI’s AI RFP Agents deliver faster drafts, centralizing knowledge and eliminating outdated content. We support vendors to respond with clarity and confidence. Our aim is to ensure proposals are compliant, competitive, and built to win.
Frequently Asked Questions
1. What are the most common types of RFPs issued in healthcare?
Healthcare RFPs frequently focus on professional services (like consulting or staffing), followed by medical or surgical equipment. Other categories include lab services, IT systems, food services, and facility maintenance. Knowing these helps vendors target their response efforts precisely.
2. Can small vendors compete effectively in healthcare RFPs?
Yes, smaller vendors can win healthcare RFPs by showcasing customized solutions, niche expertize, and personalized service. Highlighting specific success stories and responsiveness often helps them stand out against larger competitors.
3. How often should healthcare RFP requirements be updated?
Changes to RFPs are common; many include updates or clarifications mid-process. Vendors should regularly check and update their responses accordingly, such as reviewing updated Q&A or addenda weekly.
4. What framework helps structure RFP responses effectively?
A helpful method is the “why–what–how–why” format. Start with why the buyer issued the RFP, then explain what you offer, how you deliver it, and conclude with why your method ensures value. It builds clarity and alignment.
5. Should vendors share RFP pricing details with competitors?
No, pricing and proposal details should remain confidential. Sharing them with competitors breaches NDAs and compromizes fairness. It’s okay to offer general feedback, but not detailed competitor data.

90% Faster RFPs. 50% More Wins. Watch a 2-Minute Demo.
After witnessing the gap between generic AI models and the high precision required for business proposals, Gaurav co-founded Inventive AI to bring true intelligence to the RFP process. An IIT Roorkee graduate with deep expertise in building Large Language Models (LLMs), he focuses on ensuring product teams spend less time on repetitive technical questionnaires and more time on innovation.
Tired of watching deal cycles stall due to manual questionnaire back-and-forth, Dhiren co-founded Inventive AI to turn the RFP process from a bottleneck into a revenue accelerator. With a track record of scaling enterprise startups to successful acquisition, he combines strategic sales experience with AI innovation to help revenue teams close deals 10x faster.


